Stump the Shrink and how long to ban readmission for a discharged patient; indoor plants make me happy and healthy
In SAVVY, SKILLS and STUMP THE SHRINK, follow my thinking process as I ponder how to respond to a nurse practitioner’s question about how long should a program make a discharged client wait before readmitting them – 30 days, a year or what?
In SOUL, I discovered that plants and nature are good for us in almost every way you can think about. My indoor plants are not only fun to see grow and develop, but they are good for my health.
savvy, skills, and stump the shrink
Late last month, I received a question from a Nurse Practitioner (NP) that got me (DML) thinking not just about the surface question, but about the underlying assumptions of the question. So this month, I am combining SAVVY and SKILLS to address a STUMP THE SHRINK question. I’ll take you through the sequence of what was going through my head as we exchanged emails.
Here’s the original question:
Good AM Doc,
I am a practicing NP prescribing Suboxone (buprenorphine and naloxone) in Office-Based Opioid Treatment (OBOT). After a patient is being discharged from our clinic they are allowing patients to be readmitted to the clinic with no period of time to wait, sometimes the next week. Is there a period of time that patients should have to wait before being readmitted to the clinic?
Thanks.
Steve
Steven Baker, APRN_DNP (with Steve’s permission)
DML:
Here are the questions that came to mind when pondering how to respond:
- Why was the patient being discharged in the first place?
- Even if a patient was discharged, why would there have to be any “period of time to wait” if they wanted to come back?
- Was the patient being discharged for some violation of program rules; or for having a flare-up of addiction and a positive drug test for an unpresribed or illicit substance?
- I don’t think the NP would be wanting to punish a patient and ban them from treatment. Yet it sounded like the NP had bought into the notion that if a person with addiction is discharged, they have to prove they are serious about treatment before being allowed back.
- So his question is how long should the patient have to wait to be readmitted to the clinic? He is concerned that coming back the next week is too soon.
I had to get more information and see if I was right that the patient was discharged for a flare-up of addiction.
My First Response
Hi Steve:
I need some clarification. Is the patient being discharged because of substance use of non-prescribed drugs? If so, non-prescribed substance use is a poor outcome for a patient with substance use disorder. It indicates that the patient needs more assessment as to why they are not sticking to prescribed medication. Such behavior and outcomes are common in people with addiction, just as flare-ups of asthma can happen with patients who have asthma; and spikes in blood pressure for people with hypertension; and suicidal behavior in people with depression etc.
So my recommendation is not to discharge patients demonstrating poor outcomes, but rather to assess what is not going well and improve the treatment plan collaboratively with the patient, using Motivational Interviewing etc. depending on what the assessed problem(s) are.
If the patient is not interested in improving their treatment plan to learn what went wrong and chooses no further treatment, then allowing them to discharge themselves is appropriate. But If they choose to return to treatment sooner or later, there shouldn’t be a time frame banning them from services.
We should work with with them to improve their treatment plan, skills and resources to stay away from unprescribed medication or other drugs. If a patient walked away from treatment for their hypertension, depression, or asthma there wouldn’t be a time frame banning a patient to return to treatment. It should be the same for addiction.
I may have the facts all wrong on your question, so let me know more detail on your question. Hope this helps, but let me know if not.
David
NP’s First Response
Hello thanks for your reply.
I think maybe you misunderstood the question. Generally speaking, if a patient is discharged from a Medication Assisted Treatment (MAT) clinic, does that patient need to wait a certain amount of time before being readmitted?
Some clinics say 6 months. I didn’t see anything in the regulations, but if we discharge this week then allow them back the very next week, it seems like not ample time.
DML:
Here’s what went through my mind at this point:
- I don’t think I misunderstood the question. I think Steve has beliefs like lots of professionals treating addiction; judges, probation officers and Drug Court programs; and child protective service personnel: that if a person has a flare-up of addiction and uses unprescibed substances; or violates some rule of the program then the next step is some kind of sanction – suspension from treatment, some escalating behavior modification punishment; or even discharge from the program and a certain period of time to ban readmission.
- I thought of all the chronic illnesses that are caused or worsened by lifestyle choices: obesity, diabetes, hypertension, atherosclerosis and heart disease, emphysema and chronic obstructive pulmonary disease. So many of those patients do not adhere to their treatment plan, yet I have never heard of banning them from treatment if they choose to come back for services.
- How is it that an NP working in addiction has fallen into the common belief that somehow patients need to be banned from treatment for a period of time when he would never do that with these other lifestyle illnesses?
- How powerful is stigma and discrimination about addiction that an NP who would never want to punish people for their illness, appears to have been influenced by a single model of behavior modification – a model that focuses on punishment and reward; sanctions and incentives as the only approach to poor outcomes and addiction flare-ups?
- So his question remains: if a patient is discharged from a Medication Assisted Treatment (MAT) clinic does that patient need to wait a certain amount of time before being readmitted? Some clinics say 6 months…..but if we discharge this week then allow them back the very next week, it seems like not ample time.
- My question is “ample time” for what? To teach the patient a lesson for breaking rules or having poor outcomes like substance use? To sanction them into changing their behavior when we know chronic disease management works better than sanctions and punishment?
I had to get more information and see if my hunch was right. Was the patient discharged for a flare-up of addiction or some rule-breaking? I want to keep reminding the nurse practitioner that addiction is like other chronic illnesses. I want to see if I can draw on his general health experience to become aware of the powerful influence of stigma, discrimination about addiction and a behavior modification approach that permeates addiction treatment.
My Second Response
Steve, I still don’t understand the purpose of the discharge. A patient either needs MAT indefinitely to get a good outcome like a person with diabetes may need insulin indefinitely to get a good outcome. Or a person may be discharged because now s/he doesn’t need MAT because they have developed other recovery skills and are not in danger of relapse to start using again. If they find once off MAT, that it isn’t going well and they need MAT again, why would you wait to readmit them?
A person with hypertension may have normal, stabilized blood pressure and be doing well because they lost weight, stopped smoking and started an exercise program and so don’t need antihypertensive medication any more. But if their blood pressure shot up next week, and they needed medication, we wouldn’t make them wait for 6 months.
I must be missing something. Why is the person discharged off MAT? What prompts you to talk about making them wait to come back if they need it?
David
NP’s Second Response
Thank you for your response. With MAT patients who are non-compliant (missing multiple appointments, continuing use of illicit drugs, diverting medication, or using dangerous illicit drugs such as benzodiazepines etc.) – just to name a few reasons to discharge. Should we wait a period of time to readmit? Our clinic says 30 days; some clinics say a year. Wondering if there’s a regulation to speak to this?
DML:
Track my thinking from this point:
- It was what I thought all along – that the program where Steve works, like many programs, focuses on “non-compliant” behavior and then discharges patients as their response to these repeated behaviors. Then they add another sanction – a period of time to ban readmission. For some programs, as Steve says, it’s a year and for his agency, 30 days.
- By the way, “to comply” is to act in accordance with others’ wishes and with rules and regulations. When we are working to engage and attract people into recovery, treatment adherence (to cling to, to hold fast, to stick to it) is the goal not treatment compliance.
- How can I help Steve overcome the stigma and discrimination around addiction and move away from a purely behavior modification, reward and punishment approach?
- How could I remind a nurse practitioner about what healthcare professionals do with any poor outcomes in any illness? Or how to handle any patients who are not doing the most productive and wellness-producing behaviors? The next step always is to assess what is not going well and work with the patient to attract them into improving their lifestyle choices and treatment plan.
I recognized this dialogue with Steve could be a good learning opportunity for many others involved with addiction treatment. I wanted to increase awareness of how easy it is to fall under the powerful influence of stigma and discrimination about addiction and use a single behavior modification approach.
My Third Response
Steve, I plan to address your question in more detail when I write September’s edition of Tips and Topics. So I would like to use your question as a learning opportunity. How would you like to be identified or not? Let me know.
The principle I am articulating is that all the “non-compliant” behaviors you list are indicators of poor outcomes in the treatment. These are not just behavior problems that need to be sanctioned by discharge; and then further punished by making them wait to be readmitted. Any poor outcome in the treatment of any disease needs to be assessed. Depending on what is found, the patient and clinician can then collaborate on an improved treatment plan. For example, is the patient missing multiple appointments because:
- S/he has a Dimension 1 (Acute Intoxication and Withdrawal Potential, The ASAM Criteria) problem of intoxication or withdrawal symptoms;
- Or because of a flare-up of a Dimension 2 Biomedical and physical health problem like asthma or chronic pain;
- Or a Dimension 3, Emotional, Behavioral or Cognitive problem like co-occurring PTSD or anxiety disorder or depression;
- Or a Readiness to Change, Dimension 4 problem that indicates they are ambivalent about recovery thus needing motivational enhancement services;
- Or a Dimension 5, Relapse or Continued Use or Continued Problem flare-up involving use of illicit drugs. S/he doesn’t want to show up with a positive drug test because of a zero tolerance policy of sanctions for use;
- Or a Dimension 6, Recovery Environment problem with transportation, or child care or homelessness or negative, unsupportive friends.
If the patient is not interested in assessing the problems and not interested in improving the treatment plan to address what is discovered, they have a right to choose no further treatment and leave the MAT services. But if they later realize their mistakes and seek treatment again, why would you want to have a policy that turns them away, especially for a year or even 30 days?
A person with schizophrenia or bipolar disorder could miss multiple appointments and leave mental health services and then return later. Would we have a regulation that rules that the psychotic or manic person needs to wait 30 days or a year to come back to treatment?
The Bottom line is that we have come to treat addiction flare-ups and behavior as willful misconduct that needs to be punished by discharge and restriction of services. We would not do that to a person with diabetes, schizophrenia, severe depression or hypertension if they missed multiple appointments, used illicit drugs, gave their anti-anxiety or anti-depressant or antihypertensive medication to family and friends, or continued to drink or drug on top of their psychotropic medication.
Thanks for your question,
David
NP’s Third Response
Just asking questions based on situations, circumstances of our program, and witnessing practices of other providers (wanting to make sure I do things the correct way.)
Thanks,
Steve
DML:
Here are my final thoughts on Steve’s earnest question:
- Like many healthcare professionals and others involved with addiction, Steve admirably wants to “do things the correct way”. They are not out to punish people and reject them.
- But “based on situations, circumstances of our program, and witnessing practices of other providers”, it is easy to be drawn into adopting the attitudes, biases and prejuduces of society and other treatment professionals. So here are three Tips.
Be aware and beware of the stigma and discrimination about addiction that general society and even addiction treatment providers perpetuate
When a person with addiction has a flare-up and uses illicit substances; or is not adherent to treatment, if your first intervention is to sanction the person, you have succumbed to the discrimination pressures. We treat addiction flare-ups differently from how we treat flare-ups of physical and mental health.
No one thinks first to sanction a person with an asthma attack, suicidal cutting behavior, failure to take their schizophrenia or diabetes medication correctly, or a flare-up of hypertension. No one would be wanting to ban the patient from returning for care and make them wait 30 days or a year to be readmitted.
Tip 2
Behavior Modification is just one model of behavior change. It is time to broaden treatments to embrace new science of behavior change
It is easy to cling to one tried and true model of behavior modification and ignore the science of behavior change that has so many effective evidence-based practices to attract people into recovery. Motivational Intervieiwng (MI), Motivational Enhancement Therapy (MET), Twelve Step Facilitation (TSF), Cognitive Behavioral Treatment (CBT), Contingency Management (CM) in the context of recovery coaching and the list goes on.
Tip 3
There are multidimensional reasons for “non-compliant” behavior. Assess and treat poor outcomes, don’t sanction and ban treatment access
Addiction is a biopsychosocial-spiritual, chronic medical disease that has multidimensional reasons for so called “non-compliant” behavior. Such poor outcomes and behaviors need to assessed and treated, in collaboration with the patient or client.
Focusing on sanctions and regulations that restrict readmission only serves to demoralize and disincentivize a person with addiction from seeking the help they need. People with addiction are not ‘bad’ people who need to be taught a lesson and banned from treatment. They are ‘good’ people who do ‘bad’ things as part of their addiction illness.
soul
 |
I love my indoor plants, watching them sprout new shoots and leaves. It is life creating and growing before my eyes, albeit slowly. So my ears perked up when I heard an interview on Science Friday with science journalist, Emily Anthes, talking about her new book, “The Great Indoors: The Surprising Science of How Buildings Shape Our Behavior, Health, and Happiness.”
Emily indicated that we spend 90% of our lives indoors and even more during COVID. She said that indoor plants can change mood and highlighted one of the most well-validated findings in all the literature – that plants and nature are good for us in almost every way you can think about:
- They boost our mood
- Reduce stress
- Boost attention and cognitive performance
- Real house plants are good, but even fake nature, like a big photo of nature on the wall helps
- Nature sounds can have some of the same stress relieving effects.
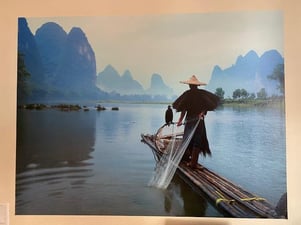
The finding that even “fake nature” and big photos of nature on the wall helps our mood was music to my ears. I sit at my desk facing a calming big photo of the Li River in southern China. Over 40 years ago, I cruised down that impressive water way lined by tall cliffs and tropical vegetation. It was a memorable, fascinating trip back then, and it keeps providing joy flowing right off my office wall.

